The first 6 to 8 weeks after giving birth are known as the postpartum period. Some recovery milestones may vary if you had a vaginal or Cesarean delivery.
During the postpartum period, which some believe lasts
These changes take place in addition to other big changes, including nursing, sleep deprivation, and the overall adjustment to parenting a newborn.
It’s not uncommon for the first year to feel like a tidal shift.
The recovery period can vary widely. If you’re on your third child and pushed for 20 minutes, your recovery will look different than if you labored for 40 hours, pushed for 3, and had an emergency C-section.
While everyone’s experience is different, there are some recovery milestones that you should ideally hit. To help give you a sense of where you should be in your postpartum timeline, we’ve highlighted what you can expect from your body and mind.
When to get medical attention
Certain symptoms in the postpartum period may indicate a need for urgent medical attention. Call 911 or seek emergency medical attention if you experience:
- chest pain
- rapid or irregular heart rate
- loss of consciousness, or passing out
- seizure
- confusion or disorientation
- coughing up blood
- feeling too tired or weak to do your usual activities
- heavy vaginal bleeding (soaking through one or more pads in an hour, or passing large blood clots, the size of an egg or larger)
- symptoms of infection, such as fever, blood in your urine, foul smelling vaginal discharge, frequent or painful urination
- thoughts of harming yourself, your baby, or someone else
Let your doctor know if you experience any other new or worsening symptoms, including:
- pain
- swelling
- headache
- dizziness or lightheadedness
- depression or anxiety
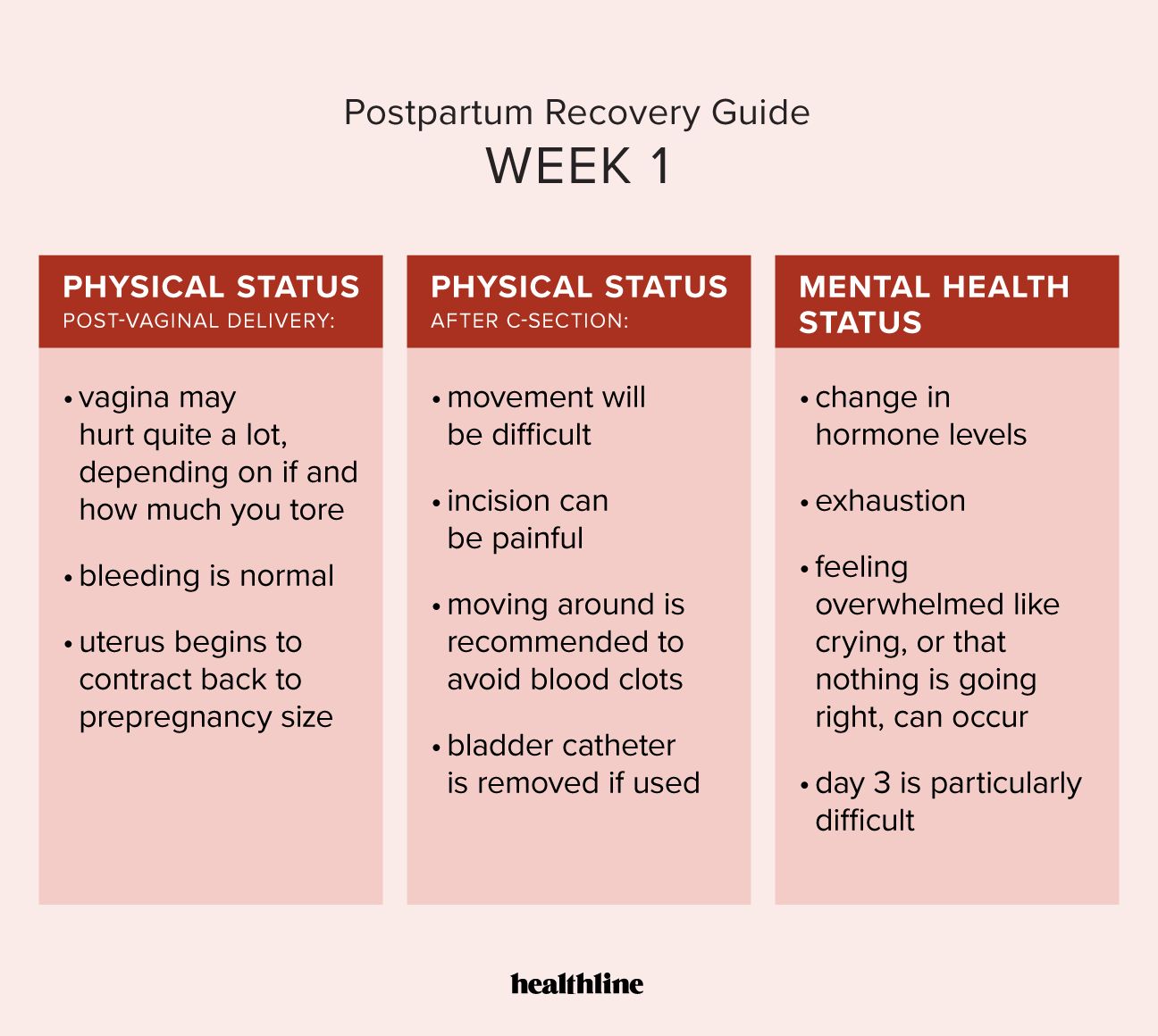
Physical status, post-vaginal delivery
If you had a hospital delivery, you’ll most likely stay there for at least part of this week after a vaginal delivery. Depending on whether or not you tore (and how much), your vagina may hurt quite a lot.
The medical term for tearing during delivery is perineal laceration, and it can affect the:
- perineum
- labia
- vagina
- cervix
- anus
Perineal soreness (soreness between the public arc and the back of the pelvis) is typical, as is bleeding.
The blood should be bright red this first week, but will eventually turn brown, similar to its appearance at the end of menstrual bleeding. You’ll also probably feel little contractions, especially when nursing as uterus contracts back to its prepregnancy size.
Physical status, after C-section
After Cesarean delivery (C-section), most movement will be difficult, and your incision can be painful. Many people have trouble getting in and out of bed, but it’s essential to move around, at least a little bit, to avoid blood clots.
If you had a bladder catheter put in, a healthcare professional will remove it.
Your uterus may also start to contract to prepregnancy size, which can cause little contractions.
Mental health status
Day 3 in particular is infamous for being emotionally challenging.
“The birth buzz is wearing off, estrogen and progesterone levels are dropping off, and prolactin and oxytocin levels rise and fall throughout the day while the baby suckles,” says Jocelyn Brown, a licensed and certified midwife in Los Angeles.
“That combined with sleep deprivation makes for lots of weepiness and feeling like nothing is going right.”
Suggestions for aiding your recovery:
- Perineum soreness and pain: If you had a vaginal delivery, use an ice pack or frozen pads with witch hazel on your perineum. Use a spray bottle of warm water during or after peeing.
- Pain medication: Take acetaminophen (Tylenol) or ibuprofen (Advil) at regular intervals. Pain begets pain, so do your best to get ahead of it.
- Stool softener: Take a stool softener and drink lots of water, which can help ease stool through your system. Many hospitals will not let you leave until you’ve pooped, so make it a little easier on yourself.
- Monitor for infection: “It’s very important to take your temperature 2 to 4 times a day for the first 72 hours,” says Brown. “We want to catch a uterine or kidney infection quickly.”
- Wound care after a C-section: Your major job the first week is to keep your incision clean and dry. Give it fresh air after a shower, pat it down with a towel, set your hair dryer to cold, and point it at your scar.
- Pelvic floor exercise: If you didn’t have pregnancy complications and your doctor says its safe to do so, you can start pelvic floor exercises to strengthen your pelvic floor muscles. This can help reduce with urinary incontinence.
Physical status, post-vaginal delivery
For some, bleeding will start to taper off during week 2, while for others, it can last up to six weeks. Both are normal.
At this point, though, the bleeding shouldn’t be heavy. You may start to feel vaginal itchiness, which is caused by the area beginning to heal. The sutures, which swell with fluid when they disintegrate, may also be uncomfortable.
“All of this often means that the wound has healed enough that [you] simply now [have] the luxury of being annoyed by the stitches because [you] is no longer in pain in that area,” says Brown. “I view the itchy-annoyed complaints as a good sign of healing.”
Physical status, after C-section
You’ll still likely feel quite sore, but it will probably feel a little easier to move around. Your scar might become a little itchy as the incision site heals.
Some doctors may clear you to drive.
Mental health status
Baby blues are normal. They affect about 39% of birthing parents in the immediate days after childbirth, but this percentage ranges from 13.7% to 76% depending on geographic location.
Postpartum depression (PPD), however, is something else entirely.
If you’re feeling overcome with sadness and anxiety, such as if you can’t eat or sleep, aren’t bonding with your newborn, or are having suicidal thoughts or thoughts of hurting yourself or anyone else, contact your doctor as soon as possible. Treatment and support are available.
PPD
Suggestions for aiding your recovery:
- Nursing pain or difficulties: If you’re nursing, you’ll be deep into it by now. Make sure to have lanolin on hand for sore nipples and watch out for clogged milk ducts. A lactation consultant can make an enormous difference here, so make sure to see one if you’re having trouble.
- Gentle exercise: Incorporate a little movement into your day, whether that’s a walk around your house or the block.
- Eating: Continue to eat well. Foods with potassium can help keep your energy up.
- Pelvic floor exercise: Continue pelvic floor exercises.
Physical status, post-vaginal delivery
This is when the uterus goes back to prepregnancy size and the bleeding stops. Most people are cleared for exercise and sexual activity, but many don’t feel ready for the latter for a long time.
“Around 6 to 8 weeks, I frequently get outreach from [people] who report that their bleeding stopped many days ago, but mysteriously started up again,” explains Brown. “This is because your uterus is involuting [shrinking] so much that the placental scab is getting pushed off, so there’s a brief few days of bright red bleeding.”
About 2 months after delivery, you may experience some hair loss or thinning, known as postpartum alopecia. It may result from changes in the hair growth cycle during pregnancy. It usually lasts about a year. Certain products for postpartum hair loss may help. Many are safe for use while nursing.
Some people may also develop urinary incontinence, or bladder leakage. This often results from weakened pelvic floor muscles. You can strengthen your pelvic floor muscles through exercises or physical therapy and use incontinence products, if you need them.
Physical status, after C-section
The uterus goes back to prepregnancy size, and most people are cleared for sex and exercise. You can now drive and lift something other than the baby, but try not to overdo it. The scar probably won’t hurt anymore, but you might still be numb (or even itchy) around the incision.
You should be fully recovered from the surgery and will probably only feel the incision if you bump into something. Walking is great, but go slow on more intense exercise.
Postpartum hair loss or thinning can also occur after a C-section.
Mental health status
If you have any worries about your emotional or mental health, bring them up with your doctor at your six-week checkup if you haven’t already.
It’s normal to feel exhausted and overwhelmed, but deeper feelings of depression, hopelessness, or anxiety may be related to PPD. Treatment can help you feel better.
Suggestions for aiding your recovery:
- Self compassion: Although this is technically when the postpartum period ends, according to the medical definition, many don’t feel remotely like themselves for a whole year, so be gentle with yourself.
- Exercise: If you’re ready to resume exercising, start slowly.
- Sex: The same holds true for sexual activity: Just because you’re cleared doesn’t mean that you feel ready. Listen to your body above all else. Sex may be painful this early after giving birth.
- Exhaustion: The exhaustion at this point can be overwhelming. Nap as often as possible.
Physical status, post-vaginal delivery
If your hair was falling out after your delivery, it may stop or lessen now, though it may continue until one year postpartum.
You may also have full bladder control again, if this was a problem before now. If not, a doctor may recommend pelvic floor exercises or therapy.
Depending on your breastfeeding schedule, your milk may be drying up.
Your period may return at anytime (or not for a year or more). This can depend on if you’re breastfeeding.
Physical status, after C-section
Just as with post-vaginal delivery, your milk may be drying up depending on your breastfeeding schedule, and your period may come back anytime.
If you experienced hair loss after your C-section, it may stop or lessen, similarly to after a vaginal delivery.
Mental health status
If you’re getting into the swing of parenthood, and your baby is sleeping more, your mental state might be more positive around this time.
Again, be sure to discuss any lingering feelings associated with PPD with a doctor or mental health professional.
Suggestions for aiding your recovery:
- Exercise: Exercise is very important at this stage for both mental and physical health. You can do abdominal strengthening exercises in earnest, which should help relieve some back pain.
- Anxiety and depression: Talk with a doctor if you’re experiencing feelings that may be related to PPD. This condition is treatable.
- Pelvic floor exercises or therapy: You can continue pelvic floor exercises. If you’re experiencing urinary incontinence, you can talk with your doctor about pelvic floor therapy.
- Sex and contraception: If you aren’t planning on becoming pregnant again, talk with your doctor about when to start contraception and when you can become pregnant again after having a baby.
Physical status, post-vaginal delivery
You may feel back to yourself, but your body may still feel slightly different, whether it’s a few extra pounds or just weight distributed in different places.
Depending on whether you’re still nursing, your breasts will appear different than in prepregnancy.
Physical status, after C-section
Your scar will have faded, but it might still be a little numb. If you want another baby soon, many doctors recommend (or insist on) a C-section if the babies are 18 months or less apart. Whether or not you can have a vaginal delivery after a C-section
Mental health status
This will probably hinge on how comfortably you’re adapting to parenthood and how much sleep you’re getting. If you can, continue to nap on weekends when the baby naps to catch up on sleep.
Suggestions for aiding your recovery:
- Ongoing complications: If you’re having painful sex, vaginal prolapse, or urinary incontinence, speak with your doctor.
- Diet and exercise: It’s important to maintain a nutritious diet and continue to exercise for your energy levels and mental health.
Abigail Rasminsky has written for the New York Times, O: The Oprah Magazine, The Cut, Lenny Letter, Longreads, and The Washington Post, among other publications. A graduate of Columbia’s MFA program, she lives in Los Angeles with her family. You can find her on her website and on X, formerly known as Twitter.